FIP in Cats: New Research, Real Cases, and What’s Working Now
Research progress on feline infectious peritonitis
FIP in Cats New Research Abstract: Feline infectious peritonitis is a systemic, fatal viral disease and one of the main causes of death in kittens and young cats. In recent years, the disease has become widespread around the world and has shown a certain upward trend. More and more scholars have studied and explored it, but its pathogenic and immune mechanisms are still not fully understood.
This article comprehensively describes feline infectious peritonitis from the aspects of etiology, pathogenesis, epidemiology, clinical symptoms, diagnosis and treatment, immunity and prevention, etc., to provide reference and guidance for the scientific diagnosis, treatment and prevention of the disease.
Keywords: Feline infectious peritonitis, epidemiology, clinical symptoms, diagnosis and treatment, prevention, feline coronavirus
FIP in Cats New Research, Real Cases, and What’s Working Now
What is FIP? The Basics
Feline infectious peritonitis (FIP) is a systemic, fatal disease of cats. Its pathogen is feline infectious peritonitis virus (FIPV), which is mutated from feline coronavirus (FCoV) [1-2]. According to different clinical manifestations, feline infectious peritonitis can be divided into three types: wet, dry, and mixed. The common clinical symptoms are depression, loss of appetite, fluctuating fever, and weight loss.
Wet FIP is mainly manifested by pleural or peritoneal effusion, while dry FIP is mainly manifested by granuloma formation in abdominal organs and lesions in the brain or eyes. When the symptoms of wet and dry FIP coexist, it is mixed FIP[3].
Currently, FIP can only be diagnosed by immunohistochemical staining to identify FCoV antigens in lesion tissues, but the operability is low and professional testing equipment and personnel are required. Therefore, it can only be diagnosed comprehensively based on medical history, clinical symptoms, laboratory diagnosis, and imaging examinations, after excluding other diseases[4].
FIP has an extremely high mortality rate and was once considered a terminal illness. In order to reduce the suffering of cats, euthanasia is recommended once the diagnosis is confirmed. In recent years, GC376, a 3C protease inhibitor, and GS-441524, a nucleoside analog, have been shown to have a certain therapeutic effect on FIP[5-8]. The author summarizes the current domestic and international research on feline infectious peritonitis and comprehensively explains and analyzes the disease in order to provide a reference for the diagnosis and treatment of the disease.
1 Etiology
Feline coronavirus is a single-stranded positive-sense RNA virus with an envelope and no segments. It is spirally symmetrical, with petal-like filaments on the surface of the envelope, and appears corona-shaped under an electron microscope[9]. FCoV belongs to the Nidovirales order, Coronaviridae family, Coronavirus genus, and is closely related to canine coronavirus and porcine transmissible gastroenteritis virus[10]. Coronavirus is the RNA virus with the largest known genome. The FCoV genome is approximately 29 kb in size and consists of 11 open reading frames (ORFs), of which two main ORFs encode a replicase; four ORFs encode structural proteins: spike protein S, envelope protein E, membrane protein M, and nucleocapsid protein N; and five ORFs encode non-structural proteins 3a, 3b, 3c, 7a, and 7b[11]. The spike protein S can be divided into two parts: the membrane fusion subunit S2, which can fix the protein on the cell envelope; and the receptor binding subunit S1, which is the main determinant of virus attachment and determines its antibody neutralization effect and serotype [12].
1.1 Biotype
There are two biotypes of feline coronavirus: one is feline enteric coronavirus (FECV), which is a ubiquitous intestinal biotype; the other is feline infectious peritonitis virus, which is a highly lethal and virulent biotype [3]. FECV usually only causes mild gastrointestinal symptoms or even no symptoms [13]. FIPV causes a systemic, immune-mediated, fatal disease, namely feline infectious peritonitis.
1.2 Serotype
Based on the virus neutralizing antibody response and the amino acid sequence of the S protein, FCoV can be divided into two serotypes: type I and type II [14]. Type I FCoV is considered to be a cat-specific strain that is dominant throughout the world but is difficult to culture in vitro. Type II FCoV, on the other hand, is a recombinant product of type I FCoV and canine coronavirus and is easier to culture in vitro, so it has been more widely studied. Type I and type II FCoV may also infect the same cat at the same time. Both FECV and FIPV biotypes have type I and type II, so the two cannot be distinguished by serotype [15].

2 Pathogenesis
Studies have shown that FECV can cause asymptomatic persistent infection, with the virus being detected in feces a few days after infection and continuing to shed for months [16]. Among cats with persistent FECV infection, approximately 5% may develop FIP [3, 17]. Sequence analysis of the two biotypes showed that the sequence similarity of FIPV and FECV strains collected from the same litter was much higher than that of FCoV sequences from different litters or regions [18].
After more experiments and analysis, scientists proposed the currently generally accepted internal mutation theory, that is, FIPV is produced by internal mutations of FECV during the continuous infection process, but it is not yet fully understood at which stage and where the mutation occurred [1-2]. At present, some studies have found that the mutation from FECV to FIPV is related to the ORF 3c gene [17], S gene [19-20] and M gene [21]. Other studies have pointed out that the loss of integrity of the ORF 7b gene (which often occurs during cell culture) will cause FIPV to lose toxicity, but it is not related to the mutation from FECV to FIPV [16, 22].
Feline infectious peritonitis virus continuously infects and replicates in monocytes and macrophages, thereby infecting systemic organs, which is a key step in the development of FIP [23]. Activated monocytes promote the expression of a large number of cytokines, such as tumor necrosis factor-α, interleukin-1β, and adhesion molecules (such as CD11b and CD18) [24], which in turn promote the interaction between monocytes and activated endothelial cells in small and medium-sized veins [25]. Activated monocytes increase the expression of certain enzymes (such as matrix metalloproteinase-9), causing endothelial barrier dysfunction, which in turn leads to monocyte extravasation [26]. Studies have also shown that vascular permeability factor produced by monocytes and macrophages infected with FIPV increases vascular permeability and fluid exudate in FIP cats [27].
Based on the presence of protein-rich exudate in the peritoneal and thoracic cavities, FIP can be divided into three clinical manifestations: wet, dry, and mixed. In natural infection, wet FIP is more common than dry and mixed FIP. The balance between cellular immunity and humoral immunity in the body largely determines the course of the disease. Cellular immunity is a protective immunity produced by the body against FIPV.
a. If the response is early and strong, FIP symptoms will not appear and the virus will not continue to proliferate.
b. If only strong humoral immunity occurs, it will develop into wet FIP. If humoral immunity is strong and accompanied by weak cellular immunity, it will develop into dry FIP.
c. If dry FIP occurs, the virus reaches the brain and eyes through monocytes, but due to the blood-brain barrier and blood-eye barrier, it is difficult for the immune response to reach these areas, so the central nervous system and eyes are more likely to develop lesions and continue to develop.
Studies have shown that the risk of FIP increases when there is dual infection or stress with feline leukemia virus and feline immunodeficiency virus. The underlying mechanism is not yet fully understood, and it may be caused by immunosuppression. In addition, unlike the highly contagious FECV [28], FIPV does not spread horizontally between cats [29]. Under experimental infection conditions, even if FIPV is detected in the feces, it will not cause FIP in the exposed cats. Therefore, FIP is sporadic and not contagious. The name “feline infectious peritonitis” is not very appropriate, but it is still used today because of habit [1, 30].
3 Epidemiology
Feline infectious peritonitis is one of the main causes of death in kittens and young cats. Wild cats and cheetahs are also susceptible animals [4]. Studies have shown that the vast majority of cats with FIP are between 3 months and 3 years old, and at least half of them are less than 1 year old. FIP can occur at any age, and there is a second peak in incidence in elderly cats (over 10 years old), which may be due to poor immune function [4].
Several studies have shown that male and unneutered cats are more likely to develop FIP [31], which may be related to the influence of sex hormone levels on the immune system. The peak of the disease may occur in autumn and winter [32]. All breeds can develop FIP, but several studies have shown that purebred cats are more susceptible, especially Abyssinian cats, Australian Mist cats, Bengal cats, Boerman cats, Burmese cats, British Shorthair cats, Himalayan cats, Ragdoll cats, Cornish Rex cats and Scottish Fold cats [4]. Breed susceptibility may vary geographically and over time, depending on the preferences of breeders and keepers in the region [3]. However, some studies have shown that FIP is not related to breed [33].
Housing density has also been considered one of the main risk factors for the development of FIP, and overcrowding may lead to viral mutation and disease progression. In addition, cats with persistent FECV infection are more likely to develop FIP due to stress, including changes in environment, food, long-distance transportation, surgery, and the addition of new pets. Stress suppresses immune function, making the virus more likely to mutate and proliferate [33].
4 Clinical signs
The clinical signs of feline infectious peritonitis tend to change over time and depend on the organs affected. The most common symptoms are depression, loss of appetite, and fluctuating fever, eventually leading to weight loss. Some cats may have increased water intake and urine output, which may be related to fever. A few cats may also develop jaundice [4]. Abdominal palpation often reveals an abdominal mass, which is presumed to be related to organomegaly or adhesions to the omentum [34].

4.1 Wet FIP
The most typical symptom of wet FIP is peritoneal effusion, which can be seen as an increase in abdominal circumference and a sense of fluid fluctuation on palpation of the abdomen. However, most owners mistakenly believe that it is caused by weight gain or pregnancy. The aspirated peritoneal fluid is yellow to varying degrees, clear or slightly turbid, and viscous. Cats with pleural effusion may experience symptoms such as dyspnea and turbid heart sounds. A few cats also develop pericardial effusion.
Studies have shown that about 10% of pericardial effusions in cats are caused by FIP, which is the third most common cause of pericardial effusion after cardiomyopathy and tumors [35]. Uncastrated male cats may develop scrotal swelling due to the spread of peritoneal inflammation and the entry of exudate into the testicular capsule. A few cats also develop systemic synovitis, which is caused by the migration of immune complexes or infected macrophages/monocytes into the synovium.
4.2 Dry FIP
Dry FIP is a chronic manifestation that occurs weeks to months after the initial infection. It is characterized by granulomas that involve abdominal organs (especially the kidneys, liver, mesenteric lymph nodes, and irregular nodules that may appear on the bowel wall), the central nervous system, and the eyes, without causing body cavity effusions [36].
Granulomatous lesions are most commonly found at the T-junction of the colon or ileocecal colon, but may also occur in the small intestine, and abdominal palpation often shows thickening of the bowel wall. Cats may develop symptoms such as chronic diarrhea, constipation, or vomiting. The most common ocular lesion is iritis [37], which manifests as a change in iris color or aqueous flare.
Some cats may develop symptoms of hyphema. In addition, FIP can cause retinal blood vessels to cuff, and occasionally suppurative granulomas may be seen. The neurological symptoms of FIP vary depending on the location and severity of the central nervous system involvement. The most common is altered mental status, followed by ataxia, then nystagmus, and other symptoms include seizures, lameness, and paralysis. The appearance of neurological symptoms indicates a poor prognosis.
When opisthotonos, rigidity of the forelimbs, and flexion of the hind limbs occur, it means that the animal is on the verge of death. A small number of cats will have non-pruritic skin lesions, mainly distributed on the neck, forelimbs, and chest wall, manifesting as well-defined, slightly raised intradermal papules [3, 38].
4.3 Mixed FIP
Mixed FIP is rare and may be a transitional stage from wet to dry or dry to wet. In the late stage of the disease, when the immune system collapses, dry FIP will also produce a large amount of exudate [3, 39]. Some cats with wet FIP may also have neurological symptoms or eye diseases.
5 Diagnostic methods

Due to the lack of specific clinical symptoms and typical biochemical and pathological abnormalities, the sensitivity and specificity of conventional detection methods are low, making it very difficult to diagnose FIP. Therefore, it is necessary to make a comprehensive diagnosis based on medical history, clinical symptoms, laboratory diagnosis, imaging examination, and histopathological examination, and after excluding other diseases. If there is coelomic exudate, analysis of the exudate can help diagnose FIP [4].
5.1 Routine blood tests
Mild non-regenerative anemia is common in cats with FIP, but severe anemia may occur. Microcytosis and low hematocrit may also occur. Lymphocytopenia is the most common hematological abnormality in both naturally infected and experimentally induced FIP [36]. It is caused by virus-induced T-cell apoptosis and exhaustion [40], and the final outcome of the disease may be related to the degree of lymphocytopenia [41]. Studies have also shown that hematocrit can better reflect the treatment process of FIP than white blood cell and lymphocyte counts [8].
5.2 Serum biochemical examination
Increased serum globulin concentration is a biochemical abnormality commonly observed in cats with FIP. This is the result of a nonspecific reaction. In particular, the increase in γ-globulin concentration has a high positive predictive value for FIP [3, 42]. Albumin concentrations often decrease, primarily due to extravasation secondary to vasculitis, but as a negative acute phase protein, levels may also decrease slightly [43]. Hyperglobulinemia can cause total protein concentrations to increase, but due to the decrease in albumin concentrations, total protein concentrations may remain normal in some cats with FIP.
In a study by Sparkes et al. [44], 50% of cats with wet FIP and 70% of cats with dry FIP had hyperproteinemia. Most studies have shown that the serum A/B ratio is more valuable for the diagnosis of FIP, and the A/B ratio of cats with FIP is significantly lower than that of normal cats. When the A/B ratio is less than 0.4, FIP is highly suspected, while when it is greater than 0.8, FIP can be basically ruled out [42]. In addition, cats with FIP may develop isolated hyperbilirubinemia, which is not associated with elevated liver enzymes. This is due to excessive destruction of red blood cells and poor glucuronidation of the cat itself, resulting in the gradual accumulation of hemoglobin breakdown products such as bilirubin and biliverdin [45].
Acute phase proteins are the products of hepatocytes in response to the acute phase response, which is the body’s early nonspecific but highly complex response to various injuries (infection, trauma, necrosis, malignant growth, etc.). FIP causes an inflammatory response, so the concentration of acute phase proteins will increase.
The main test items for cats are serum amyloid A (SAA), α1-acid glycoprotein (AGP), and haptoglobin (Hp). In a study on the role of acute phase proteins in the differential diagnosis of FIP and other diseases that cause body cavity effusion in cats, Hazuchova et al. [46] found that AGP was better than SAA and Hp in differential diagnosis, with a sensitivity and specificity of 93%. However, the concentrations of the above three acute phase proteins in certain diseases (such as sepsis and diffuse tumors) are no different from those of FIP, so none of them can be used as a single diagnostic indicator for FIP. The study by Giori et al. [47] showed that although AGP cannot be used alone to confirm FIP, when FIP is highly suspected and cannot be confirmed by autopsy and clinical pathology, an elevated AGP concentration can support the diagnosis of FIP.
5.3 Reverse transcription-polymerase chain reaction
There are many reports on the detection of FCoV using reverse transcription-polymerase chain reaction (RT-PCR). Some primers designed for conserved regions of the viral genome, such as the 3′-untranslated region (3′-UTR)[48] and the 7b gene[49], can detect most FCoV strains. The S gene sequence is different between the two serotypes of FCoV, so some RT-PCR detection methods use the S gene as a target to distinguish FCoV serotypes[50]. Studies have shown that the S gene of FCoV contains two amino acid substitutions, M1058L and/or S1060A, which correspond to the nucleotide mutations 23,531 A>T/C and 23,537 T>G, respectively, which can be used to distinguish whether it is FIPV infection or FECV infection[19, 51].
Therefore, related commercial diagnostic tests designed based on this principle have begun to be used in clinical diagnosis in recent years. However, some studies have shown that the analysis of S gene mutations in FCoV does not significantly improve the ability to diagnose FIP compared with the detection of FCoV alone. This is because the above mutations are not caused by FIP, but by the systemic spread of FCoV [52]. Real-time fluorescence quantitative RT-PCR is currently also used to detect FIP pathogens [53]. Virus quantification is valuable for distinguishing between systemic infection and intestinal infection, because the viral load of systemic infection is much higher. This method can be used to detect whether cats with negative serology but FIP symptoms contain the virus, and can also be used for shedding detection in epidemiological studies.
Because the specific genetic factors of FCoV biotypes are unknown and the genome contains multiple single nucleotide polymorphisms, RT-PCR can only detect FCoV strains and cannot distinguish between FECV and FIPV. False negative results may occur when the virus count is low or when RNA is degraded during sample transportation. Therefore, the RT-PCR detection method has great limitations. A positive result does not necessarily mean that the patient has FIP, and a negative result cannot rule out FIP [54]. Studies have shown that the detection of FCoV in exudates, aqueous humor, and lesion tissues has a greater diagnostic value for FIP, while the detection of blood, feces, and cerebrospinal fluid is not very meaningful [4, 34].
5.4 FCoV antibody level detection
FCoV antibody levels can be detected by immunofluorescence antibody detection, enzyme-linked immunosorbent assay, and virus neutralization test. Different laboratories use different detection methods, resulting in large differences in results [55]. Like RT-PCR, FCoV antibody level detection is only for FCoV, but cannot determine whether it is FIPV. The study of Meli et al. [56] showed that in virus-rich samples, FCoV antibody level detection may also have false negatives. This may be due to the combination of virus particles in the sample with antibodies, resulting in extremely low detection levels or even undetectable.
In addition, since antibodies are not produced until 18 to 21 days after infection with FCoV, if the test is performed too early after exposure to the virus, it will also result in false negative results. When quarantine or purification of cats for FCoV, it is very useful to measure antibody levels. If the test method is sensitive enough, a negative result for FCoV antibodies in a clinically healthy cat means that the cat is not infected.
5.5 Exudate analysis
The exudate of cats with FIP is yellow to varying degrees, clear or slightly turbid, and viscous, and may contain fibrin clots. The exudate has a high protein content (greater than 3.5 g·dL-1) and contains a small number of nucleated cells (less than 5,000 cells per microliter), usually mildly degenerated neutrophils and macrophages.
If the fluid is bloody, purulent, chylous, or foul-smelling, the possibility of FIP is very small. Determination of protein concentration in the exudate also has certain diagnostic value. When the white-to-globulin ratio is greater than 0.8, FIP can almost be ruled out; when the white-to-globulin ratio is between 0.45 and 0.8, it may be FIP; when the white-to-globulin ratio is less than 0.45, it is very likely to be FIP[57].
Total nucleated cell count (ΔTNC) is performed by an automated hematology analyzer (Sysmex XT-2000iV, Sysmex Europe, Norderstedt, Denmark) and has a high diagnostic accuracy for FIP. The ΔTNC values of cats with FIP are much higher than those of healthy cats. When the reference cutoff value is set at 1.7, the diagnostic sensitivity is 79% to 90% and the specificity is 94% to 100%. When the reference cutoff value is set at 2.5 or 3.4, the specificity increases to 100% [58-59].
The Rivalta test is a simple test method that can distinguish between exudate and transudate. Add 8 mL of distilled water to a transparent test tube or measuring cylinder (volume 10 mL), add a drop of 98% acetic acid and shake to mix, then drop a drop of body cavity fluid into it. If the drop quickly dissipates in the solution and the solution remains clear, the result is negative; if the drop maintains its shape, stays on the liquid surface, or slowly descends like a jellyfish, the result is positive [60].
FIP exudates are not only high in protein but also contain high concentrations of fibrinogen and inflammatory mediators, which can result in positive results. A study by Fischer et al. [61] showed a sensitivity of 91.3%, a specificity of 65.5%, a positive predictive value of 58.4%, and a negative predictive value of 93.4% for FIP. These values increase when diseases such as lymphoma and bacterial infection are excluded or when only cats less than 2 years of age are considered. Given its good sensitivity and negative predictive value, the Rivalta test should be included in the routine evaluation of every FIP cat with exudate [62].
Immunofluorescence staining of macrophages in the exudate for infection with FCoV (with both negative and positive controls) confirms the diagnosis of FIP. Although FCoV may be present in healthy cats, only macrophages in FIP cats contain sufficient amounts of antigen to result in positive staining. However, false-negative results may occur when insufficient numbers of infected cells are present, when viral load is too low, or when antigen cannot be detected due to antibody binding [42].
5.6 Imaging Studies
In wet FIP, the volume of exudate may be small and difficult to detect in the early stages of the disease. At this time, ultrasound or radiology can be used to identify or confirm the presence of exudate and assist in collecting samples [45]. Abdominal ultrasound findings in cats with FIP may include: anechoic or mildly echoic peritoneal effusion; hyperechoic masses in the mesentery; hypoechoic abdominal lymphadenopathy; diffuse or focal hypoechoic liver and spleen enlargement; medullary signs in the kidneys [63], increased cortical echogenicity, hypoechoic nodules and subcapsular effusions; and thickening of the bowel wall or intestinal mass lesions. Thoracic ultrasound through the diaphragm may reveal pleural effusions or comet tail artifacts due to pulmonary infiltrates [64].
Chest radiographs in feline infectious peritonitis may show: pleural effusions; enlarged cardiac contours in cats with pericardial effusions; pulmonary nodules or peribronchial infiltrates in cats with suppurative granulomatous pneumonia. Abdominal radiographs may show loss of peritoneal or retroperitoneal detail due to peritoneal effusion, hepatomegaly, splenomegaly, nephromegaly, and mass lesions in the gastrointestinal tract or abdominal lymph nodes [4].
5.7 Histopathological Examination
At necropsy, gross pathological findings in cats with FIP may include: varying degrees of peritoneal, pleural, or pericardial effusion; fibrinous adhesions; mesenteric masses; diffuse or focal bowel wall thickening or mass lesions; enlarged or irregular abdominal organs and thoracic and/or abdominal lymphadenopathy; multifocal, miliary, nodular lesions (granulomas) of varying sizes that are white, creamy, yellow, or brown in color, either within the parenchyma or on the serosal surfaces of organs such as the kidneys, liver, spleen, pancreas, and lungs; lesions may also be present in the nasal cavity and paranasal sinuses; examination of the brain may reveal fibrous exudates in the meninges with or without ventricular dilatation and hydrocephalus. Lesions may be more severe in cases of dry FIP. The histopathological manifestations of FIP are mainly systemic vasculitis and purulent granulomatous lesions. The lesions mainly include an increase in macrophages and neutrophils, with fewer lymphocytes and plasma cells. Gangrene may occur in the lesions. In addition, pathological changes such as purulent granulomatous meningoencephalomyelitis, choroiditis, membranous glomerulonephritis, and lymphocyte failure have also been reported.
Immunohistochemical staining is the gold standard for diagnosing FIP and is used to show whether the virus is present in the damaged tissue, but this method can only be performed in professional laboratories. Because cat tissues are sticky and often bind non-specifically to irrelevant antibodies, non-FCoV antibodies must be used as controls. Lack of controls will result in false positive results. However, it is very difficult to safely and effectively collect samples of lesion tissue from sick cats, and this invasive diagnostic method is difficult for owners to accept, so the diagnosis of FIP remains a difficult problem for clinical veterinarians [3-4, 34-45].
6 Treatment
Feline infectious peritonitis was once considered a terminal illness. Currently, there is no effective treatment. Only some drugs can be used to prolong life and improve quality of life [65]. Prednisolone can temporarily relieve the clinical symptoms of cats with FIP. Immunosuppressants such as chlorambucil and cyclophosphamide have also been used, but the side effects and prognosis are still unclear. Some researchers have also tried a variety of immunomodulators and antiviral drugs, such as ribavirin and human recombinant interferon α, but there is no convincing in vivo experimental support [4].
Other reported drugs include pentoxifylline (immunomodulator), polyisoprene (immunostimulant), ozagrel hydrochloride (thromboxane synthase inhibitor), and nelfinavir (antiviral drug), all of which require further clinical control trials to evaluate their effectiveness and safety. Small interfering RNA molecules and cyclosporine A have been shown to inhibit FIPV replication in in vitro experiments, but whether they are effective for clinical FIP cats remains to be determined [66].
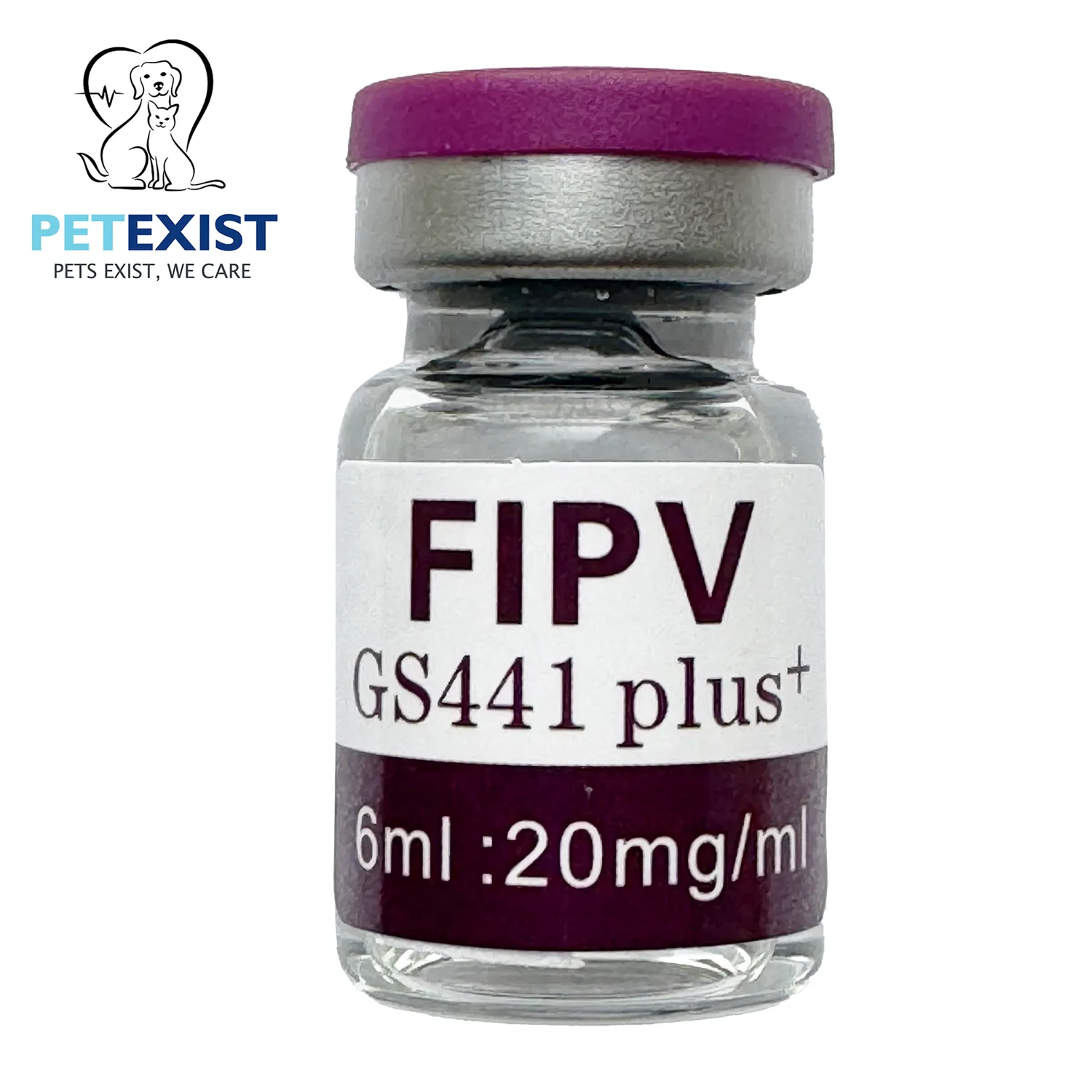
In recent years, research on drugs for the treatment of FIP has been continuously updated. A 3C protease inhibitor (GC376) has been shown to have a good effect on experimentally infected FIP cats. Although it can achieve a certain degree of relief for naturally infected cats, there are still many relapses [5, 7]. Subsequently, a nucleoside analog (GS-441524) was found to be safe and effective in treating naturally infected FIP by directly interfering with the replication process of the virus encoding [6, 8].
Regarding the comparison of the efficacy of GC376 and GS-441524, two studies by Pedersen et al. [7-8] showed that the cure rate of GS-441524 seemed to be higher, and it was still effective for FIP cats with neurological symptoms and had no obvious adverse reactions. However, GC376 could not cure cats that already had neurological symptoms and might affect the development of permanent teeth in young cats. Since the treatment regimens and dosages of the two in the experiment were different, it cannot be concluded that GS-441524 is absolutely more effective than GC376.
According to the results of these two studies, the optimal therapeutic dose of GC376 is 15 mg·kg-1, subcutaneously injected, once every 12 hours; the optimal therapeutic dose of GS-441524 is 4 mg·kg-1, subcutaneously injected, once a day. The treatment time of both should be at least 12 weeks. At present, GS-441524 is widely used in the clinical treatment of FIP. Considering the economic cost, the recommended dose is 2~4 mg·kg-1, and the treatment should be continued for at least 4 weeks.
Then, based on the results of routine clinical examinations and laboratory tests, professional veterinarians decide whether to stop or continue treatment. In addition, appropriate and reasonable supportive treatment and dietary management are essential. Due to the high price of existing therapeutic drugs, long treatment cycles, and the possibility of recurrence after drug withdrawal, complete cure of FIP is still rare [67-68].
7 Immunization and prevention
Many scientists have tried to develop FIP vaccines, but most have failed because antibody-dependent enhancement was observed during the experiment, resulting in more cats developing FIP after vaccination than in the control group. Currently, there is only one vaccine (Primucell, Pfizer Animal Health, New York), which is used in the United States and some European countries and is administered intranasally. It contains a temperature-sensitive type II FCoV mutant DF2-FIPV. However, the protective efficacy of this vaccine is controversial, given that type I FCoV is more prevalent worldwide [69].
Although cats infected with FCoV do not necessarily develop FIP, it is still necessary to eliminate the transmission route and avoid contact between other cats and FIP cats. If a cat in the household has died of FIP, it is recommended that owners wait at least two months before getting a new cat, so that all FCoV in the environment can be inactivated. At the same time, any factors that may have caused the previous cat to become ill should be identified and addressed, such as environmental changes, overcrowding, and fright.
In addition, before introducing a new cat to an environment, the FCoV infection status of existing cats and new cats should be determined. Only by purging FCoV can the source of FIP be eliminated [32]. Paying attention to environmental hygiene, preventing overcrowding, maintaining a high ratio of adult cats to juvenile cats, and ensuring that the number of cats in each room is stable at 3 or less can reduce the risk of disease transmission. Some studies have shown that FIP is breed-specific. Further exploration of the genetic factors that cause FIP and selective breeding can reduce the risk of the disease [69].
8 Outlook
With the development of the economy and the improvement of people’s living standards, the number of pet cats is increasing, and the incidence of feline infectious peritonitis is also increasing year by year. Feline infectious peritonitis is a highly lethal disease that seriously threatens the health of cats and affects the lives of pet owners. At present, the pathogenesis and immune mechanism of feline infectious peritonitis are not yet fully understood, and there is a lack of specific diagnostic methods and accurate and effective therapeutic preparations. We believe that as scientists and veterinary workers pay more attention to and conduct in-depth research on feline infectious peritonitis, the pathogenesis and diagnosis and treatment methods of the disease will be updated faster, and conquering the disease is just around the corner;
At the same time, the research on the mutation mechanism of feline infectious peritonitis virus also provides a reference for the research of other species of coronaviruses.
References:
| [1] | BANK-WOLF B R, STALLKAMP I, WIESE S, et al. Mutations of 3c and spike protein genes correlate with the occurrence of feline infectious peritonitis[J]. Vet Microbiol, 2014, 173(3-4): 177–188. |
| [2] | LEWIS C S, PORTER E, MATTHEWS D, et al. Genotyping coronaviruses associated with feline infectious peritonitis[J]. J Gen Virol, 2015, 96(6): 1358–1368. |
| [3] | PEDERSEN N C. A review of feline infectious peritonitis virus infection: 1963-2008[J]. J Feline Med Surg, 2009, 11(4): 225–258. |
| [4] | SYKES J E. Canine and feline infectious diseases[M]. Amsterdam: Elsevier Science, 2013: 195-208. |
| [5] | KIM Y, LIU H W, KANKANAMALAGE A C G, et al. Reversal of the progression of fatal coronavirus infection in cats by a broad-spectrum coronavirus protease inhibitor[J]. PLoS Pathog, 2016, 12(3): e1005531. |
| [6] | MURPHY B G, PERRON M, MURAKAMI E, et al. The nucleoside analog GS-441524 strongly inhibits feline infectious peritonitis (FIP) virus in tissue culture and experimental cat infection studies[J]. Vet Microbiol, 2018, 219: 226–233. |
| [7] | PEDERSEN N C, KIM Y, LIU H W, et al. Efficacy of a 3C-like protease inhibitor in treating various forms of acquired feline infectious peritonitis[J]. J Feline Med Surg, 2018, 20(4): 378–392. |
| [8] | PEDERSEN N C, PERRON M, BANNASCH M, et al. Efficacy and safety of the nucleoside analog GS-441524 for treatment of cats with naturally occurring feline infectious peritonitis[J]. J Feline Med Surg, 2019, 21(4): 271–281. |
| [9] | TANG X J, WANG S, YIN Y Y, et al. Statistical analysis on cases of feline infectious peritonitis in an animal clinic in Wuhan city of Hubei province[J]. China Animal Health Inspection, 2019, 36(4): 22–25. (in Chinese) |
| [10] | GONZÁLEZ J M, GOMEZ-PUERTAS P, CAVAN-AGH D, et al. A comparative sequence analysis to revise the current taxonomy of the family Coronaviridae[J]. Arch Virol, 2003, 148(11): 2207–2235. |
| [11] | KIPAR A, MELI M L. Feline infectious peritonitis:still an enigma?[J]. Vet Pathol, 2014, 51(2): 505–526. |
| [12] | MYRRHA L W, SILVA F M F, DE OLIVEIRA PETERNELLI E F, et al. The paradox of feline coronavirus pathogenesis:a review[J]. Adv Virol, 2011, 2011: 109849. |
| [13] | MALBON A J, MELI M L, BARKER E N, et al. Inflammatory mediators in the mesenteric lymph nodes, site of a possible intermediate phase in the immune response to feline coronavirus and the pathogenesis of feline infectious peritonitis?[J]. J Comp Pathol, 2019, 166: 69–86. |
| [14] | SHIBA N, MAEDA K, KATO H, et al. Differentiation of feline coronavirus type Ⅰ and Ⅱ infections by virus neutralization test[J]. Vet Microbiol, 2007, 124(3-4): 348–352. |
| [15] | TILLEY L P, SMITH JR F W K. Blackwell’s five-minute veterinary consult: canine and feline[M]. Ames, Iowa: John Wiley and Sons, 2016. |
| [16] | TEKES G, THIEL H J. Feline coronaviruses:pathogenesis of feline infectious peritonitis[J]. Adv Virus Res, 2016, 96: 193–218. |
| [17] | CHANG H W, DE GROOT R J, EGBERINK H F, et al. Feline infectious peritonitis:insights into feline coronavirus pathobiogenesis and epidemiology based on genetic analysis of the viral 3c gene[J]. J Gen Virol, 2010, 91(2): 415–420. |
| [18] | PEDERSEN N C, BOYLE J F, FLOYD K, et al. An enteric coronavirus infection of cats and its relationship to feline infectious peritonitis[J]. Am J Vet Res, 1981, 42(3): 368–377. |
| [19] | CHANG H W, EGBERINK H F, HALPIN R, et al. Spike protein fusion peptide and feline coronavirus virulence[J]. Emerg Infect Dis, 2012, 18(7): 1089–1095. |
| [20] | LICITRA B N, MILLET J K, REGAN A D, et al. Mutation in spike protein cleavage site and pathogenesis of feline coronavirus[J]. Emerg Infect Dis, 2013, 19(7): 1066–1073. |
| [21] | BROWN M A, TROYER J L, PECON-SLATTERY J, et al. Genetics and pathogenesis of feline infectious peritonitis virus[J]. Emerg Infect Dis, 2009, 15(9): 1445–1452. |
| [22] | DEDEURWAERDER A, DESMARETS L M, OLYSLAEGERS D A J, et al. The role of accessory proteins in the replication of feline infectious peritonitis virus in peripheral blood monocytes[J]. Vet Microbiol, 2013, 162(2-4): 447–455. |
| [23] | PEDERSEN N C, LIU H W, SCARLETT J, et al. Feline infectious peritonitis:role of the feline coronavirus 3c gene in intestinal tropism and pathogenicity based upon isolates from resident and adopted shelter cats[J]. Virus Res, 2012, 165(1): 17–28. |
| [24] | MALBON A J, FONFARA S, MELI M L, et al. Feline infectious peritonitis as a systemic inflammatory disease:contribution of liver and heart to the pathogenesis[J]. Viruses, 2019, 11(12): 1144. |
| [25] | REGAN A D, COHEN R D, WHITTAKER G R. Activation of p38 MAPK by feline infectious peritonitis virus regulates pro-inflammatory cytokine production in primary blood-derived feline mononuclear cells[J]. Virology, 2009, 384(1): 135–143. |
| [26] | KIPAR A, MAY H, MENGER S, et al. Morphologic features and development of granulomatous vasculitis in feline infectious peritonitis[J]. Vet Pathol, 2005, 42(3): 321–330. |
| [27] | TAKANO T, OHYAMA T, KOKUMOTO A, et al. Vascular endothelial growth factor (VEGF), produced by feline infectious peritonitis (FIP) virus-infected monocytes and macrophages, induces vascular permeability and effusion in cats with FIP[J]. Virus Res, 2011, 158(1-2): 161–168. |
| [28] | ADDIE D, HOUE L, MAITLAND K, et al. Effect of cat litters on feline coronavirus infection of cell culture and cats[J/OL]. J Feline Med Surg, 2019: 1-8. [2020-03-04]. https://journals.sagepub.com/doi/pdf/10.1177/1098612X19848167. |
| [29] | STRANIERI A, PROBO M, PISU M C, et al. Preliminary investigation on feline coronavirus presence in the reproductive tract of the tom cat as a potential route of viral transmission[J]. J Feline Med Surg, 2020, 22(2): 178–185. |
| [30] | TEKES G, SPIES D, BANK-WOLF B, et al. A reverse genetics approach to study feline infectious peritonitis[J]. J Virol, 2012, 86(12): 6994–6998. |
| [31] | WORTHING K A, WIGNEY D I, DHAND N K, et al. Risk factors for feline infectious peritonitis in Australian cats[J]. J Feline Med Surg, 2012, 14(6): 405–412. |
| [32] | FOLEY J E, POLAND A, CARLSON J, et al. Risk factors for feline infectious peritonitis among cats in multiple-cat environments with endemic feline enteric coronavirus[J]. J Am Vet Med Assoc, 1997, 210(9): 1313–1318. |
| [33] | RIEMER F, KUEHNER K A, RITZ S, et al. Clinical and laboratory features of cats with feline infectious peritonitis-a retrospective study of 231 confirmed cases (2000-2010)[J]. J Feline Med Surg, 2015, 18(4): 348–356. |
| [34] | GREENE C E. Infectious diseases of the dog and cat[M]. Saunders-Elsevier, 2010: 92-108. |
| [35] | DAVIDSON B J, PALING A C, LAHMERS S L, et al. Disease association and clinical assessment of feline pericardial effusion[J]. J Am Anim Hosp Assoc, 2008, 44(1): 5–9. |
| [36] | NORSWORTHY G D. The feline patient[M]. West Sussex: John Wiley & Sons, 2018: 181-183. |
| [37] | HUANG X, HOU Z Y, LI H Y, et al. Diagnosis of nonexudative feline infectious peritonitis in[J]. Chinese Journal of Veterinary Medicine, 2018, 54(12): 84–85. (in Chinese) |
| [38] | REDFORD T, AL-DISSI A N. Feline infectious peritonitis in a cat presented because of papular skin lesions[J]. Can Vet J, 2019, 60(2): 183–185. |
| [39] | PEDERSEN N C. An update on feline infectious peritonitis:virology and immunopathogenesis[J]. Vet J, 2014, 201(2): 123–132. |
| [40] | VERMEULEN B L, DEVRIENDT B, OLYSLAEGERS D A, et al. Suppression of NK cells and regulatory T lymphocytes in cats naturally infected with feline infectious peritonitis virus[J]. Vet Microbiol, 2013, 164(1-2): 46–59. |
| [41] | PEDERSEN N C, ECKSTRAND C, LIU H W, et al. Levels of feline infectious peritonitis virus in blood, effusions, and various tissues and the role of lymphopenia in disease outcome following experimental infection[J]. Vet Microbiol, 2015, 175(2-4): 157–166. |
| [42] | HARTMANN K, BINDER C, HIRSCHBERGER J, et al. Comparison of different tests to diagnose feline infectious peritonitis[J]. J Vet Intern Med, 2003, 17(6): 781–790. |
| [43] | CERÓN J J, ECKERSALL P D, MARTÍNEZ-SUBIELA S. Acute phase proteins in dogs and cats:current knowledge and future perspectives[J]. Vet Clin Pathol, 2005, 34(2): 85–99. |
| [44] | SPARKES A H, GRUFFYDD-JONES T J, HARBOUR D A. An appraisal of the value of laboratory tests in the diagnosis of feline infectious peritonitis[J]. J Am Anim Hosp Assoc, 1994, 30: 345–350. |
| [45] | PEDERSEN N C. An update on feline infectious peritonitis:diagnostics and therapeutics[J]. Vet J, 2014, 201(2): 133–141. |
| [46] | HAZUCHOVA K, HELD S, NEIGER R. Usefulness of acute phase proteins in differentiating between feline infectious peritonitis and other diseases in cats with body cavity effusions[J]. J Feline Med Surg, 2017, 19(8): 809–816. |
| [47] | GIORI L, GIORDANO A, GIUDICE C, et al. Performances of different diagnostic tests for feline infectious peritonitis in challenging clinical cases[J]. J Small Anim Pract, 2011, 52(3): 152–157. |
| [48] | DUARTE A, VEIGA I, TAVARES L. Genetic diversity and phylogenetic analysis of Feline Coronavirus sequences from Portugal[J]. Vet Microbiol, 2009, 138(1-2): 163–168. |
| [49] | KENNEDY M A, ABD-ELDAIM M, ZIKA S E, et al. Evaluation of antibodies against feline coronavirus 7b protein for diagnosis of feline infectious peritonitis in cats[J]. Am J Vet Res, 2008, 69(9): 1179–1182. |
| [50] | BENETKA V, KVBBER-HEISS A, KOLODZIEJEK J, et al. Prevalence of feline coronavirus types Ⅰ and Ⅱ in cats with histopathologically verified feline infectious peritonitis[J]. Vet Microbiol, 2004, 99(1): 31–42. |
| [51] | LONGSTAFF L, PORTER E, CROSSLEY V J, et al. Feline coronavirus quantitative reverse transcriptase polymerase chain reaction on effusion samples in cats with and without feline infectious peritonitis[J]. J Feline Med Surg, 2017, 19(2): 240–245. |
| [52] | BARKER E N, STRANIERI A, HELPS C R, et al. Limitations of using feline coronavirus spike protein gene mutations to diagnose feline infectious peritonitis[J]. Vet Res, 2017, 48: 60. |
| [53] | GUAN X T, LI H, HAN M J, et al. Epidemiological investigation of feline infectious peritonitis in cats living in Harbin, Northeast China from 2017 to 2019 using a combination of an EvaGreen-based real-time RT-PCR and serum chemistry assays[J]. Mol Cell Probes, 2020, 49: 101495. |
| [54] | FELTEN S, WEIDER K, DOENGES S, et al. Detection of feline coronavirus spike gene mutations as a tool to diagnose feline infectious peritonitis[J]. J Feline Med Surg, 2017, 19(4): 321–335. |
| [55] | PRATELLI A. Comparison of serologic techniques for the detection of antibodies against feline coronaviruses[J]. J Vet Diagn Invest, 2008, 20(1): 45–50. |
| [56] | MELI M L, BURR P, DECARO N, et al. Samples with high virus load cause a trend toward lower signal in feline coronavirus antibody tests[J]. J Feline Med Surg, 2013, 15(4): 295–299. |
| [57] | SHELLY S M, SCARLETT-KRANZ J, BLUE J T. Protein electrophoresis on effusions from cats as a diagnostic test for feline infectious peritonitis[J]. J Am Anim Hosp Assoc, 1988, 24(5): 495–500. |
| [58] | GIORDANO A, STRANIERI A, ROSSI G, et al. High diagnostic accuracy of the Sysmex XT-2000iV delta total nucleated cells on effusions for feline infectious peritonitis[J]. Vet Clinic Pathol, 2015, 44(2): 295–302. |
| [59] | STRANIERI A, PALTRINIERI S, GIORDANO A. Diagnosing feline infectious peritonitis using the Sysmex XT-2000iV based on frozen supernatants from cavitary effusions[J]. J Vet Diagn Invest, 2017, 29(3): 321–324. |
| [60] | TASKER S. Diagnosis of feline infectious peritonitis:update on evidence supporting available tests[J]. J Feline Med Surg, 2018, 20(3): 228–243. |
| [61] | FISCHER Y, SAUTER-LOUIS C, HARTMANN K. Diagnostic accuracy of the Rivalta test for feline infectious peritonitis[J]. Vet Clin Pathol, 2012, 41(4): 558–567. |
| [62] | FELTEN S, HARTMANN K. Diagnosis of feline infectious peritonitis:a review of the current literature[J]. Viruses, 2019, 11(11): 1068. |
| [63] | FERREIRA A, MARWOOD R, BATCHELOR D, et al. Prevalence and clinical significance of the medullary rim sign identified on ultrasound of feline kidneys[J]. Vet Rec, 2019. [2020-03-04]. https://veterinaryrecord.bmj.com/content/early/2019/11/20/vr.105619.full. |
| [64] | LEWIS K M, O’BRIEN R T. Abdominal ultrasonographic findings associated with feline infectious peritonitis:a retrospective review of 16 cases[J]. J Am Anim Hosp Assoc, 2010, 46(3): 152–160. |
| [65] | WANG G L, WANG Y, DAI J T, et al. Advances in research on feline infectious peritonitis[J]. Heilongjiang Animal Science and Veterinary Medicine, 2018(7): 62–65. (in Chinese) |
| [66] | ZHANG X Y. Treatment of feline infectious peritonitis[J]. Chinese Journal of Traditional Veterinary Science, 2019(3): 89–95. (in Chinese) |
| [67] | JIANG J C, WANG Z H, ZHANG S Y, et al. Diagnosis of a case of feline infectious peritonitis[J]. Heilongjiang Animal Science and Veterinary Medicine, 2018(8): 125–235. (in Chinese) |
| [68] | MAO J F, XIE Q R, XIA Z F. Clinical changes and outcome of 146 cases of cats with feline infectious peritonitis[J]. Animal Husbandry & Veterinary Medicine, 2019, 51(10): 122–126. (in Chinese) |
| [69] | ADDIE D, BELÁK S, BOUCRAUT-BARALON C, et al. Feline infectious peritonitis:ABCD guidelines on prevention and management[J]. J Feline Med Surg, 2009, 11(7): 594–604. |








Reviews
There are no reviews yet.